Left Atrial Appendage Closure Device

By Brian H. Sarter, M.D., F.A.C.C., F.H.R.S.
Atrial fibrillation is the most common arrhythmia encountered in practice today and affects over 33 million people worldwide. One of the most devastating complications of atrial fibrillation is stroke. During atrial fibrillation, the atria (top chambers of the heart) do not contract normally and the blood pools inside the atria increasing the risk of clot development. If these clots migrate from the heart to the brain, a stroke develops. A patient with atrial fibrillation is five times more likely to develop a stroke over their lifetime. In light of this risk, most patients with atrial fibrillation are prescribed anticoagulants (blood thinner). Currently there are two major types of anticoagulants—Warfarin (Coumadin) and the Novel Oral Anticoagulants (NOAC). The three most common NOACs prescribed in the United States are Pradaxa, Eliquis and Xarelto. Both Warfarin and the NOACs provide good protection against strokes due to clots but have increased risks of bleeding and other side effects. While these medications reduce the risk of strokes due to clots, they can increase the risk of a bleeding stroke. Furthermore, many patients find anticoagulants to be inconvenient and costly. Randomized trials of Warfarin and the NOACs demonstrate that roughly 20-28% of patients end up discontinuing their anticoagulant therapy. The risk of major bleeds on these medications ranges from 2.1-3.6% per year.
Based on these limitations, significant research has been dedicated to develop a non-pharmacological approach to stroke prevention in patients with atrial fibrillation. Several studies have demonstrated that in patients with atrial fibrillation not due to valvular heart disease (vast majority of patients) over 90% of the clots that develop come from the left atrial appendage. The left atrial appendage is a sack-like projection attached to the top left chamber (figure). The Watchman Left Atrial Appendage Closure device (figure) is the first FDA approved alternative to long-term anticoagulation therapy for stroke prevention in patients with non-valvular atrial fibrillation. This device is delivered percutaneously through the femoral veins (in the leg) and implanted directly into the left atrial appendage effectively occluding this structure and preventing clot formation. The procedure takes approximately 90 minutes and requires that the patient stay overnight in the hospital. At the end of the procedure, the patient has only a small bandage over the puncture wound in the femoral vein. The risk of complication from the procedure is 3-4%.
The Watchman device was evaluated in five clinical studies involving more than 2,400 patients and nearly 6,000 patient years of follow-up. This device was compared to warfarin therapy and demonstrated comparable stroke risk reduction. Importantly, when compared with warfarin, the Watchman device resulted in an 85% reduction in hemorrhagic (bleeding) stroke, 63% reduction in disabling stroke, and 56% reduction in cardiovascular death over long-term follow-up. After 45 days, most patients with the Watchman device were able to stop taking warfarin and over 99% were off warfarin at 1 year. The Watchman device was approved for sale in Europe in 2005 and in some countries in Asia in 2009. It was approved for commercial use in the United States in March, 2015 and greater than 10,000 devices have been implanted worldwide.
The ideal candidate for consideration of Watchman implantation is a patient with non-valvular atrial fibrillation felt to be at high risk for thromboembolic (clotting) strokes, who has had significant bleeding complications from anticoagulation therapy or is deemed high risk for future bleeds. Pre-procedure assessment requires a screening transesophageal echocardiogram (TEE) to assess the left atrial appendage size and shape. Patients will need to be on warfarin prior to the procedure and then at least for 45 days after the procedure. At 45 days, a repeat TEE is performed and if this demonstrates good occlusion of the left atrial appendage, warfarin can be discontinued. Patients are then treated with aspirin and plavix (two anti-platelet drugs) for 6 months then aspirin alone.
While most patients with atrial fibrillation can be managed effectively with warfarin or NOACs, there is an important subgroup of patients in whom anticoagulation is felt to be too high risk. The Watchman device is a first-of-its-kind, proven alternative for these patients. This simple device implanted minimally invasively can truly be life-changing for these patients.
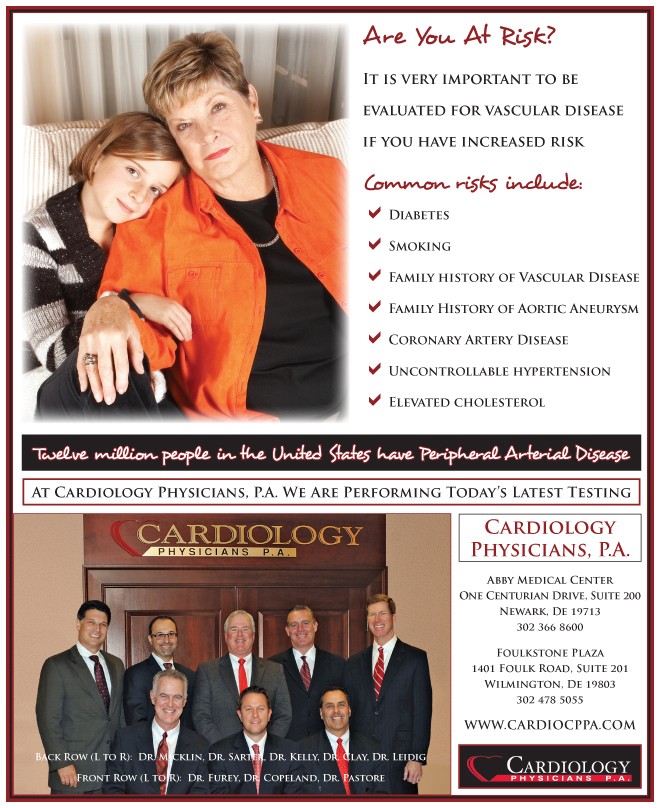
For more information please visit our website at www.cardiocppa.com or call us at 302)478-5055.
Dr. Brian H. Sarter has been a member of Cardiology Physicians since April 1998. Dr. Sarter attended Duke University where he graduated Summa Cum Laude with his Bachelor’s Degree in Science. He attended the New York University School of Medicine where he was elected to Alpha Omega Alpha (Medical Honor Society). He completed his Internal Medicine training at the Hospital of the University of Pennsylvania. He continued at the Hospital of the University of Pennsylvania to complete two years of his Cardiology fellowship and did additional training in the subspecialty of Electrophysiology at Hahnemann University Hospital and Medical College of Pennsylvania. Dr. Sarter has authored or co-authored over 30 papers in the field of Electrophysiology which have been published in major Cardiology Journals. He is a Fellow of the Heart Rhythm Society and American College of Cardiology and a member of the Delaware Medical Society.
Dr. Sarter has a strong commitment to clinical and consultative Cardiology and his added expertise in Electrophysiology allows our Practice to service the needs of patients with cardiac rhythm disturbances. Dr. Sarter has extensive experience in both medical and interventional treatment of cardiac arrhythmias. He is highly proficient in defibrillator implantation, pacemaker therapy, and radiofrequency ablation of both ventricular and atrial dysrhythmias. He is the first physician in the community to have implanted biventricular pacing devices for the treatment of chronic refractory congestive heart failure and the first physician in the community to offer curative catheter ablation for atrial fibrillation. Dr. Sarter is the Medical Director of the Heart and Vascular Interventional Services and the Associate Chief of Cardiology at ChristianaCare Hospital in Newark, Delaware.
Dr. Sarter and his wife Eileen were married in 1991 and have two children, Jake and Darian. Dr. Sarter enjoys spending time with his family as well as jogging, golfing, skiing and exercise.