Preventing Stroke in Patients with Atrial Fibrillation: It’s not just Coumadin anymore
By Brian H. Sarter, M.D., F.A.C.C., F.H.R.S.
Thromboembolic complications, primarily stroke, is the most concerning consequence of atrial fibrillation (AF). AF increases the risk of stroke 4-5 fold and is responsible for 15-20% of all ischemic strokes. Without therapy, the risk of ischemic strokes in patients with AF is 5% per year. Until recently, the only option for preventing strokes in patients with AF was either aspirin or warfarin therapy (Coumadin). While aspirin does confer some protection against stroke, early trials demonstrated that warfarin therapy is clearly superior. The SPAF-II trial (Stroke Prevention in Atrial Fibrillation II) demonstrated that compared with aspirin, warfarin reduced the risk of stroke 27-33% depending on age group. The BAFTA trial (Birmingham Atrial Fibrillation Treatment of the Aged) demonstrated a 52% risk of stroke and arterial embolism in patients treated with warfarin vs. aspirin.
Despite this proven benefit, many patients with atrial fibrillation (under 60% of eligible patients) are not treated with warfarin. Difficulty with compliance with blood draws, risk of bleeding, dietary restrictions, difficulty in achieving therapeutic INR levels, patient preference, and concerns regarding interactions with other medications are common reasons why eligible patients are not receiving warfarin. Thus, for > 50 years, patients and clinicians have been awaiting the arrival of newer oral anticoagulants.
Since October of 2010, the FDA has approved three new oral anticoagulants which have dramatically changed the way patients with atrial fibrillation are treated. These new oral anticoagulants are direct thrombin (dabigatran-Pradaxa) and factor Xa inhibitors (rivaroxaban-Xarelto and apixaban-Eliquis). Many trials involving large numbers of patients demonstrated the benefits of these drugs prior to approval. Dabigatran was the first drug approved and was evaluated in the RE-LY trial in which it was compared with warfarin in 18,113 patients with non-valvular AF. At a dose of 150 mg twice daily, dabigatran reduced the risk of stroke or systemic embolism by 35% compared to warfarin as well as reducing the risk of hemorrhagic stroke. There was no difference in the risks of major bleeding between the two drugs. Rivaroxaban was evaluated in the ROCKET-AF trial which randomized 14,264 patients with atrial fibrillation to rivaroxaban 20 mg daily or dose adjusted warfarin. For the primary endpoint of stroke and non-cerebral embolism, Rivaroxaban proved to be non-inferior to warfarin. Treatment with rivaroxaban did result in a statistically significant reduction of intracranial hemorrhage. The ARISTOTLE trial, compared apixaban (5 mg twice daily) to warfarin in 18,201 AF patients. In patients treated with apixaban, the rate of the primary outcome of ischemic or hemorrhagic stroke or systemic embolism was reduced 21%. Treatment with apixaban also reduced the rate of major bleeding by 31% and the risk of death from any cause by 11% compared with treatment with warfarin.
Taken together, these data demonstrate that all three of these agents provide at least as good or superior protection from stroke compared to warfarin while leading to a similar or reduced risk of major bleeding. Furthermore, these drugs are easier to take in that they do not require any blood test monitoring, show limited adverse interaction with other medications, require no dietary restrictions, provide a more consistent level of anticoagulation and have a shorter onset of action (typically 24-48 hours). However, there are some significant drawbacks to these drugs. All of these medications are more expensive than warfarin and all of them should not be used in patients with significant renal dysfunction. Most importantly, at this time there is no known antidote to reverse the effects of these medications, making the management of patients who present with acute bleeds or need for acute surgery challenging.
Since there have been no head to head comparisons between these three drugs, it is very difficult to recommend which one is superior. Unlike twice daily dabigatran and apixaban, rivaroxaban allows for once per day dosing, but of the three drugs, it was the only one that did not demonstrate improved rates of stokes and embolism compared with warfarin. Like all decisions in medicine, the choice of anticoagulation agent needs to be individualized. Hopefully, the availability of these drugs will lead to increased use of anticoagulation in patients with atrial fibrillation in order to avoid the devastating consequence of a stroke.
Brian H. Sarter, M.D., F.A.C.C., F.H.R.S.
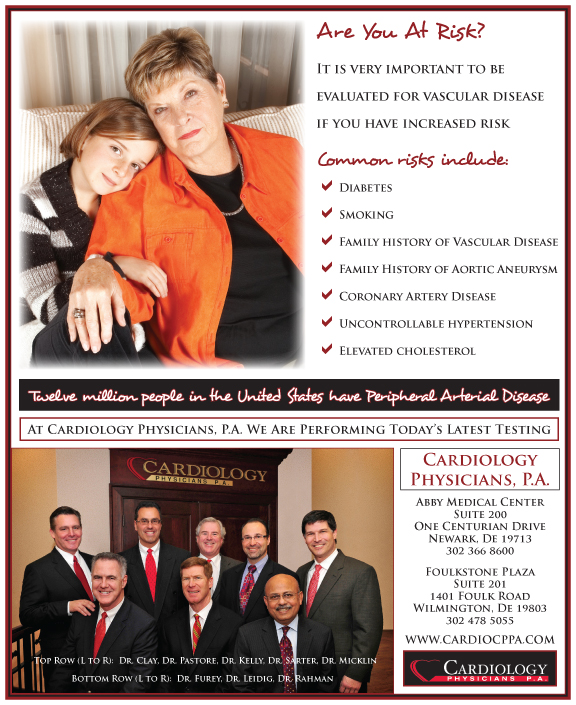
Dr. Brian H. Sarter has been a member of Cardiology Physicians since April 1998. Dr. Sarter attended Duke University where he graduated Summa Cum Laude with his Bachelor’s Degree in Science. He attended the New York University School of Medicine where he was elected to Alpha Omega Alpha (Medical Honor Society). He completed his Internal Medicine training at the Hospital of the University of Pennsylvania. He continued at the Hospital of the University of Pennsylvania to complete two years of his Cardiology fellowship and did additional training in the subspecialty of Electrophysiology at Hahnemann University Hospital and Medical College of Pennsylvania. Dr. Sarter has authored or co-authored over 30 papers in the field of Electrophysiology which have been published in major Cardiology Journals. He is a Fellow of the Heart Rhythm Society and American College of Cardiology and a member of the Delaware Medical Society.
Dr. Sarter has a strong commitment to clinical and consultative Cardiology and his added expertise in Electrophysiology allows our Practice to service the needs of patients with cardiac rhythm disturbances. Dr. Sarter has extensive experience in both medical and interventional treatment of cardiac arrhythmias. He is highly proficient in defibrillator implantation, pacemaker therapy, and radiofrequency ablation of both ventricular and atrial dysrhythmias. He is the first physician in the community to have implanted biventricular pacing devices for the treatment of chronic refractory congestive heart failure and the first physician in the community to offer curative catheter ablation for atrial fibrillation. Dr. Sarter is the Medical Director of the Heart and Vascular Interventional Services and the Associate Chief of Cardiology at ChristianaCare Hospital in Newark, Delaware.
Dr. Sarter and his wife Eileen were married in 1991 and have two children, Jake and Darian. Dr. Sarter enjoys spending time with his family as well as jogging, golfing, skiing and exercise.