COVID19 & Ophthalmology – The Past, Present & Future
By Paula Ko, MD
Looking back on the last year, the pandemic has forced us to learn, change, and grow as an Ophthalmology community, private practice, and as individuals. COVID19 is far from over, but this article looks to review how we have responded over the past year, and where we still must go.
Last March, we were faced with an emerging pandemic that the medical community had to respond to quickly. I found that Delaware’s public health system strived to stay transparent and open with the decisions they were making. The hospitals shut down all elective surgeries, routine medical exams and many medical/cancer screenings were put on hold, and some cancer treatments were delayed. As President of the Delaware Academy of Ophthalmology, I tried to bring our Ophthalmology community together to support one another, and learn from each other. We discussed how to handle each medical or business situation we were dealt, and made decisions by assimilating and distilling as much new and changing information as possible.
Many practices donated PPE (personal protective equipment) to hospitals who were dealing directly with infected SARS-CoV-2 patients, however much of it had to be used for ourselves and our staff. During eye exams, doctors and technicians are very close to patients and need to be protected. In March of 2020, it was still unclear how infectious the virus was to our staff, and how well masks prevented infection. It turned out that masks were one of our greatest weapons in stopping transmission in the office.
While each practice handled their medical patients differently, the vast majority of the Ophthalmology offices stayed open to care for patients who had ongoing vision threatening issues. Routine eye exams and refractions were all cancelled. Almost all cataract surgeries were cancelled, as well as non-emergent glaucoma, plastic, cornea and retina surgery. We painstakingly looked at patients’ charts and saw the ones who we thought could not wait such as: patients with macular degeneration and diabetic retinopathy who needed injections to preserve vision, patients with acute vision loss who needed to be evaluated and possibly treated, patients with eye pain from trauma who could not wait. Only emergency surgeries were performed, such as retinal detachments or acute glaucoma. Many people did not feel comfortable venturing inside a doctor’s office or hospital and as a result, our volume dropped by greater than 80%.
Another major issue we all dealt with was keeping our employees as “whole” as possible. Remember, private practices are also small businesses. We felt responsible to our dedicated employees to continue to pay them as much as we could, as well as keep them safe. The back-office employees started to work from home as we quickly changed our phone and computer systems to connect from their homes. Ophthalmic technicians who felt comfortable coming into the office were protected with masking, face shields, plexiglass around equipment and air purification. Patients were also screened for symptoms at the front door and had to wait in their cars until they were ready to be seen. The PPP loans and Health and Human service loans were instrumental in keeping us afloat. Some employees continued working and some were furloughed until the volume of patients started to increase again. By the end of 2020 we were able to hire back almost all of our employees as we started seeing more patients. It was a stressful time for all, as were also addressing home issues such as child care, online school and care of elderly family members.
By playing a role in my home, child’s high school, private practice, Ophthalmology and medical communities, I felt like I was making a very small dent in the way things were handled. I was encouraged to see many of my colleagues reach out past their comfort zone and attempt to help our greater Delaware community via testing, organizing, teaching, listening and learning to help defeat the SARS-CoV-2 virus. I am also encouraged to see this happening as our medical community works to vaccinate as many as possible in Delaware.
There have been many lessons learned through the past year and we will continue to educate ourselves as the fight to defeat the SARS-CoV-2 virus is not over. In 2021 our Ophthalmology practice is looking to open up our offices fully and safely, and be more proactive rather than reactive. Most all employees are now back working in the office, as long as their child care needs are met. We will encourage our patients to get vaccinated, allow them to sit socially distanced inside our offices, allow family members to come in the office (especially if vaccinated!), be more efficient in how we see them (such as doing bilateral injections on patients so they don’t have to come in twice), continue with telehealth options and expand at-home testing as technology increases this capability. As we reopen our offices to full capacity, I encourage everyone to not forget the other things we learned during COVID19 – appreciating the simplicity and beauty of close relationships, family, and downtime.
For more information call 302-652-3353 or visit www.eyephysicians.com
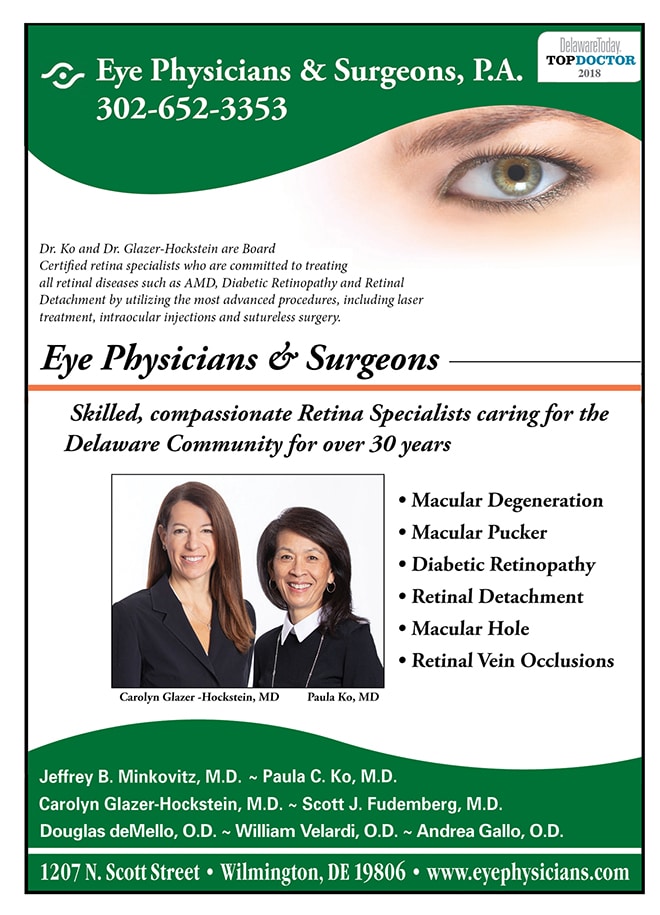
About Dr. Paula Ko
Dr. Ko graduated Cum Laude from the Ohio State University College of Engineering and received her M.D. degree from the Ohio State University College of Medicine, with honors. Following her residency in Ophthalmology at Temple, Dr. Ko served a prestigious fellowship at Georgetown University in diseases of the retina and vitreous and is Certified by the American Board of Ophthalmology. Dr. Ko’s area of expertise is in retinal problems, especially diabetic eye disease, macular degeneration, and retinal detachment. She lectures extensively and has published many papers on these topics. Dr. Ko is active in resident training and is on staff at Temple University, as well as at the Medical Center of DE. She is at the forefront of ophthalmic technology, and utilizes the most advanced procedures, including laser treatment, suture-less surgery and intraocular injections, in the care of her patients.
About Dr. Glazer-Hockstein
Dr. Glazer-Hockstein graduated Cum Laude from Jefferson Medical College. She was a member of the Hobart Armory Hare Honor Medical Society and was elected to the Alpha Omega Alpha Honor Society. She also received the Carol R. Mullen prize in ophthalmology. She completed her residency at the Scheie Eye Institute, University of Pennsylvania. During that time she was elected Chief Resident. After residency, Dr. Glazer-Hockstein completed a two years medical retina fellowship at the Scheie Eye Institute, University of Pennsylvania. She has published multiple articles in peer-review journals and has lectured on a variety of retinal disease subjects. Her specialization includes but is not limited to: macular degeneration, retinal vascular disease, and diabetic retinopathy.