Understanding The Connection Between Diabetes And Vision Loss
By Dr. Carolyn Glazer-Hockstein, MD
Patients with diabetes may suffer from a group of conditions, which together are called diabetic eye disease. This includes diabetic retinopathy, cataract (clouding of the lens inside the eye) and glaucoma (a group of diseases that damage the optic nerve) Diabetic retinopathy occurs in more than half of patients affected by diabetes. It is the leading cause of blindness in working age Americans. Both type 1 and type 2 diabetics are equally affected by blindness.
Diabetic retinopathy is the term that describes damage to the vessels of the retina. The retina is a thin layer of light-sensitive nerve tissue that lines the back of the eye. When light enters the eye it passes through the iris to the retina where images are focused and converted into electrical impulses. These electrical signals are carried by the optic nerve to the brain and give us vision.
Elevated glucose (sugar) in the blood causes damage to small blood vessels in the retina. The sugar eats away at the walls of the blood vessels. The damaged vessels leak fluid (swelling) in the center of the retina that provides the sharp vision needed for reading and recognizing faces. This is known as diabetic macular edema.
Damaged blood vessels limit circulation or oxygen delivery to the retina. The blood vessels carry nutrition to the delicate retinal nerve tissue. With impaired oxygen delivery, the retina releases growth factors that cause abnormal new blood vessels to grow on the surface of the retina. This is known as proliferative diabetic retinopathy. The new fragile, abnormal blood vessels bleed and cause scar tissue formation. This may lead to retinal detachment.
Both diabetic macular edema and proliferative diabetic retinopathy may lead to blindness.
Who is at greatest risk for developing diabetic retinopathy? The longer someone has the diabetes, the greater the risk of developing diabetic retinopathy. Other risk factors for developing diabetic retinopathy include: poor control of blood sugar levels over time, high blood pressure, high cholesterol, and pregnancy.
What are the symptoms of diabetic retinopathy? Many people do not have symptoms until the disease is very advanced. Symptoms may include: blurred vision, difficulty reading, new floaters, a shadow across the vision, eye pain or pressure, and decreased color vision.
The best way to diagnose diabetic retinopathy is a dilated ophthalmologic exam. Yearly examinations for diabetics are extremely important to look for retinal changes that may occur before a patient has symptoms. If diabetic retinopathy is discovered, often more frequent examinations are required to monitor for advancement of the disease.
Additional testing also helps detect and manage diabetic retinopathy. An optical coherence tomography (OCT) study is a valuable non-invasive test, which is frequently used to evaluate retinal thickness and to assist in the detection of retinal swelling. This test helps to determine whether fluid has leaked into the retina and it also helps track response to treatment.
Fundus photographs (a photograph of the retina and optic nerve) provide documentation of retinal changes and helps physicians monitor the disease.
Fluorescein angiography is a specific test that evaluates the retinal blood vessel circulation. This is a test in which the physician injects a dye into the patient’s arm. The dye circulates through the body to the eye and the photographer takes pictures. The fluorescein highlights the retinal blood vessels allowing the physician to determine whether the blood vessels are closed, damaged, or leaking. The fluorescein angiogram also provides a map and can help guide treatment.
There are fortunately many effective treatments for diabetic retinopathy. Treatment may include intravitreal injections (small injections of medication into the eye), laser treatment, and vitreous and retinal surgery. These treatments can prevent, treat, or reverse damage from diabetes in the retina.
The National Eye Institute has advised the way to keep your vision is by keeping your health on TRACK:
• Take your medicines as prescribed by your doctor
• Reach and maintain a healthy weight
• Add physical activity to your day
• Control your ABCs (A1C, blood pressure, and cholesterol)
• Kick the smoking habit
Prevention and early detection with regular eye examinations helps maintain vision for diabetic patients. Understanding how and why diabetic retinopathy occurs empowers patients to take control and save their eyesight.
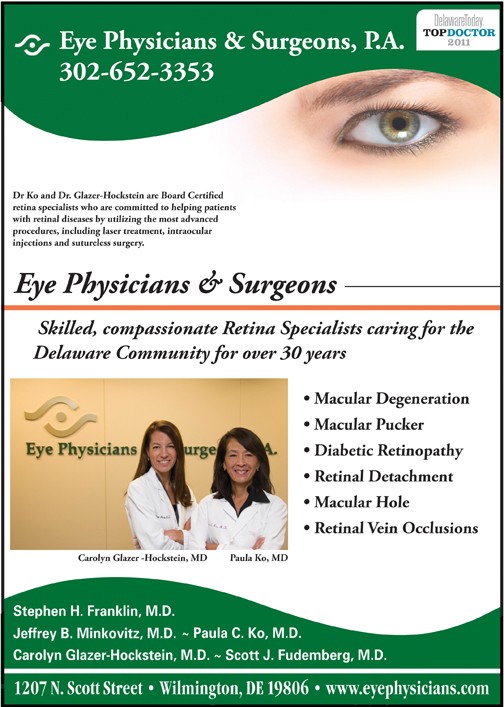
Dr. Glazer-Hockstein graduated Cum Laude from Jefferson Medical College. She was a member of the Hobart Armory Hare Honor Medical Society and was elected to the Alpha Omega Alpha Honor Society. She also received the Carol R. Mullen prize in ophthalmology. She completed her residency at the Scheie Eye Institute, University of Pennsylvania. During that time she was elected Chief Resident. After residency, Dr. Glazer-Hockstein completed a two years medical retina fellowship at the Scheie Eye Institute, University of Pennsylvania.
Dr. Glazer-Hockstein has published multiple articles in peer-review journals and has lectured on a variety of retinal disease subjects. Her specialization includes but is not limited to: macular degeneration, retinal vascular disease, and diabetic retinopathy.
Paula C. Ko, MD is with Eye Physicians & Surgeons, P.A., 1207 North Scott Street, Wilmington, DE 19806. Dr. Ko graduated with honors from the Ohio State University College of Engineering in 1984. Dr. Ko received her M.D. degree from the Ohio State University College of Medicine in 1989, again with honors. Following her residency in Ophthalmology at Temple, Dr. Ko served a prestigious fellowship at Georgetown University in diseases of the retina and vitreous, and is Certified by the American Board of Ophthalmology.
Dr. Ko has an area of special expertise in retinal problems, especially diabetic eye disease, macular degeneration, retinal detachment, and CMV retinitis. Dr. Ko has lectured extensively, and has published many papers on these topics. Dr. Ko is active in resident training, and is on staff at the University of MD and Temple University, as well as at the Medical Center of DE. Dr. Ko is at the forefront of ophthalmic technology, and utilizes the most advanced procedures, including laser treatment and intraocular injections, in the care of her patients.