Ocular Tumors: Choroidal Nevus Vs. Choroidal Melanoma
By Dr. Paula Ko, MD
There are many types of tumors that can be seen in the eye. Some are benign (not cancerous) and some are malignant (cancerous). In an adult, the most common benign tumor found in the eye is a choroidal nevus and the most common primary malignant tumor is a choroidal melanoma. These tumors can be diagnosed by an eye doctor with a dilated eye exam. Having a nevus can lead to melanoma in the future so it is important that a patient is aware of this initial diagnosis and returns for frequent follow up visits with their eye doctor.
CHOROIDAL NEVUS – Benign
A choroidal nevus is like a “mole” in the back of the eye. It is located behind the retina, in the choroid, and can only be diagnosed on a dilated eye exam. It is more common in patients with fair skin and light colored irides. So for example, a patient with blond hair, blue or green eyes and fair skin is more likely to have a nevus then is someone with dark hair, dark skin and brown eyes. The pigment tends to have a protective effect. This is the same for a mole on the skin. People who are fair-skinned, are at a higher risk for skin cancer from moles than people who are dark-skinned, just like they are more at risk for a choroidal nevus to turn into a melanoma in the eye.
A nevus (freckle) is usually diagnosed on a routine dilated exam by your eye doctor. It doesn’t cause any visual symptoms and if it doesn’t convert to melanoma, will not cause problems in the eye. The pupils must be dilated in order to diagnose. If you are diagnosed with a nevus in the eye then you should do the following:
1. Always wear a hat or visor when out in the sun to protect your eyes from UV light.
2. Always wear sunglasses that block both UVA and UVB light.
3. Have a UV coating protection placed on your regular glasses.
4. Be aware that glass blocks UV light, so staying inside but getting the warmth and light from the sun keeps you safe from UV radiation if behind glass.
5. Always get your eyes dilated and examined every 6 months by your eye doctor for the rest of your life as a nevus can convert to melanoma and you will not be aware until it gets large and affects vision
When you see a mole on your skin, most people know they must check it regularly and if it is growing in size and or changing in shape they know they need to get it checked by a dermatologist. Unfortunately it is impossible for someone to monitor their own choroidal nevus as it can not be seen by the naked eye. A patient must be dilated and examined with special equipment every 6 months. Just because vision is good doesn’t mean the the nevus is not growing or not converting to a melanoma. A melanoma must be relatively large before it starts affecting vision. This 6 month check should be done for the rest of a patient’s life.
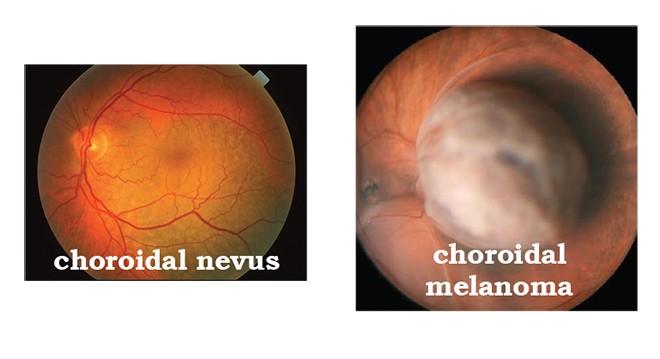
CHOROIDAL MELANOMA – Malignant
If a patient is diagnosed with a melanoma, luckily there is successful treatment if caught early. Choroidal melanomas are usually treated with Plaque Radiation which requires the patient to have surgery. A plaque that has radioactive seeds is sewn onto the sclera (the outer back layer) in the location of the tumor. It is attached to the sclera and the plaque remains there for a few days and then is removed. The radiation alone is enough to treat the lesion and regress the tumor. Sometimes if the melanoma is too big then the entire eyeball needs to be enucleated (taken out) but these cases are rare as usually patients are diagnosed before the tumor grows too large. If the tumor has metastasized (seeded to other locations in the body), the patient will need to get chemotherapy in order to treat lesions in the body. The most common place for a choroidal melanoma to travel to is the lungs and liver. The prognosis for someone who has metastatic lesions to other organs is very poor.
Once treatment is done with plaque radiation the vision is affected and gets worse, but not always. It depends on the size and location of the tumor. Vision may go down initially or over the years from the long term side effects of the radiation.
The overall prognosis for someone who has a choroidal melanoma is guarded and is usually dependent on the size of the tumor when diagnosed and the type of the cells found on biopsy. The prognosis can be good if treated early. The mortality rate is not as high as skin melanoma but is still a very serious cancer. Some studies show that about 30-50% of patients with choroidal melanoma die within 10 years of diagnosis. Before cancer treatment is initiated, patients will have blood tests and body scans to see if the tumor has spread, especially to the lungs and liver. Once a patient is treated they will be checked every 6 months to check for tumor spread. These types of tests can be done by their primary care physician or oncologist in follow up.
Facts to know about Choroidal Melanoma
1. Occurs in about 6 people in 1 million population.
2. More commonly seen in fair-skinned, light irides, light haired population.
3. Most commonly seen around age 55 but can occur in young adults and the elderly.
4. Extremely rare in the African American population.
5. Initially most patients are asymptomatic and their vision is good.
6. Symptoms may include blurred vision, flashes, floaters or a scotoma (partial loss of vision) when the tumor gets bigger.
SUMMARY
A choroidal nevus is benign and should be be checked every 6 months for the rest of a a patient’s life to make sure that it doesn’t turn into a choroidal melanoma. A Choroidal melanoma is malignant and can be be treated successfully, most effectively when the a tumor is found small and early in the disease process. Just because a patient’s vision is is “good” doesn’t mean they do not have a nevus or a melanoma. Patients should always be checked for this during their routine dilated eye exams.
Dr. Glazer-Hockstein graduated Cum Laude from Jefferson Medical College. She was a a member of the Hobart Armory Hare Honor Medical Society and was elected to the Alpha Omega Alpha Honor Society. She also received the Carol R. Mullen prize in ophthalmology. She completed her residency at at the Scheie Eye Institute, University of of Pennsylvania. During that time she was elected Chief Resident. After residency, Dr. Glazer-Hockstein completed a two years medical retina fellowship at the Scheie Eye Institute, University of Pennsylvania.
Dr. Glazer-Hockstein has published multiple articles in peer-review journals and has lectured on a variety of retinal disease subjects. Her specialization includes but is not limited to: macular degeneration, retinal vascular disease, and diabetic retinopathy.
Paula C. Ko, MD is with Eye Physicians & Surgeons, P.A., 1207 North Scott Street, Wilmington, DE 19806. Dr. Ko graduated with honors from the Ohio State University College of Engineering in 1984. Dr. Ko received her M.D. degree from the Ohio State University College of Medicine in 1989, again with honors. Following her residency in Ophthalmology at Temple, Dr. Ko served a prestigious fellowship at Georgetown University in diseases of the retina and vitreous, and is Certified by the American Board of Ophthalmology.
Dr. Ko has an area of special expertise in retinal problems, especially diabetic eye disease, macular degeneration, retinal detachment, and CMV retinitis. Dr. Ko has lectured extensively, and has published many papers on these topics. Dr. Ko is active in resident training, and is on staff at the University of MD and Temple University, as well as at the Medical Center of DE. Dr. Ko is at the forefront of ophthalmic technology, and utilizes the most advanced procedures, including laser treatment and intraocular injections, in the care of her patients.
Dr. Carolyn Glazer-Hockstein and Dr. Paula Ko are retina specialists at Eye Physicians
and Surgeons who are committed to taking care of patients with all retinal diseases. If you would like to schedule an appointment or get a second opinion please call (302) 652-3353.