Macular Pucker
By Paula C. Ko, MD
The following article is the first part of a three part series about macular diseases: Macular Pucker, Macular Hole and Macular Degeneration. These are 3 separate clinical diseases that all affect the macula but have different causes and different treatments. Patients commonly confuse the three diseases because they all affect the macula. This article will be about Macular Pucker.
Macular Pucker is a condition of the retina that can cause distortion and blurred central vision. Other names for this idiopathic disease include epiretinal membrane or pre-retinal membrane.
The macula is the center part of the retina that allows one to read, drive, and recognize people’s faces. It controls the central vision. Even though the name of this disease is “macular pucker”, it not the same thing as “macular degeneration.” They are two completely separate diseases with different etiologies.
Macular pucker is not as common as macular degeneration but it is not uncommon. It is more prevalent in patients as they age, but can also be found in younger patients. Many times the disease is idiopathic (don’t know why one gets it) but sometimes it can be related to trauma, eye inflammation, and sometimes diabetes. Patients may have a macular pucker and not even be aware, if it is mild.
The disease is not always progressive so if there are no symptoms then no treatment is recommended.
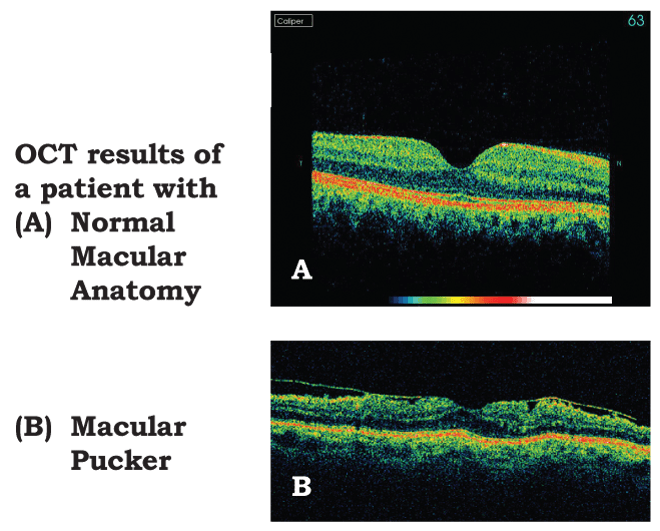
It is caused by very fine scar tissue (membrane) that lines the inner (top) layer of the macula. Usually the macular anatomy is nice and smooth with a gentle dip in the middle called the foveal dip. This is where the light focuses on the retina when a patient looks directly at something, giving them very fine precise vision. The anatomy is altered by the fine scar tissue growing on the retina, causing the area to wrinkle. Instead of a nice smooth surface with a gentle dip, the surface can be corrugated and elevated by the scar. As a result the patient’s fine vision is altered. They may complain of distortion, which means that straight lines look crooked or wavy. There also be a blur in the center of the vision. The peripheral (or side vision) is usually no affected. This anatomic change can occur in one or both eyes. If it is only in one eye, the best way to determine if a patient is symptomatic is to check vision one eye at a time. If both eyes are open, sometimes one is not aware of distortion, central blurring or decreased vision because the good eye takes over.
Treatment for macular pucker involves outpatient surgery in the operating room. A patient would need a pars plana vitrectomy procedure that requires 3 small sutureless incisions in the sclera (the white part of the eye), which gently removes the vitreous jelly in the eye as well as the fine scar tissue that lines the inner layer of the retina. Sometimes the membrane is so fine we need to stain the tissue in surgery with a special dye to see it as we operate. Preoperatively, a special test called OCT (Optical Coherent Tomography) can measure the extent of the membrane. The OCT is used to gauge the extent of the disease and to look at the detailed anatomy before and after surgery. Most times a patient sees better after the surgery. The visual acuity improves and the anatomy changes to a smoother surface allowing the patient to read much easier. If a patient is bothered with his or her vision, especially if they are having problems reading or driving then surgical intervention is recommended. If a patient is not bothered by the distortion and is functioning fine with the vision that they have, then the macular pucker should just be monitored. The patient can do this monitoring at home with an Amsler grid, which will help objectively map out their distortion. If there are any significant changes on the Amsler grid, the patient is counseled to call their doctor for an examination. Macular puckers do not tend to progress quickly so this is not an emergent situation if more distortion is noted.
In summary, Macular Pucker can be successfully repaired surgically in symptomatic patients. This surgery is done on an outpatient basis and vision usually improves slowly over a 6 week to 6-month period. This disease is not related to macular degeneration and does not increase the risk of this disease.
Paula C. Ko, MD is with Eye Physicians & Surgeons, P.A., 1207 North Scott Street, Wilmington, DE 19806. Dr. Ko graduated with honors from the Ohio State University College of Engineering in 1984. Dr. Ko received her M.D. degree from the Ohio State University College of Medicine in 1989, again with honors. Following her residency in Ophthalmology at Temple, Dr. Ko served a prestigious fellowship at Georgetown University in diseases of the retina and vitreous, and is Certified by the American Board of Ophthalmology.
Dr. Ko has an area of special expertise in retinal problems, especially diabetic eye disease, macular degeneration, retinal detachment, and laser and intraocular injections. Dr. Ko has lectured extensively, and has published many papers on these topics.
Dr. Ko is active in resident training, and is on staff at the University of MD and Temple University, as well as at the Medical Center of DE. Dr. Ko is at the forefront of ophthalmic technology, and utilizes the most advanced procedures, including laser treatment and intraocular injections, in the care of her patients.
Dr. Carolyn Glazer-Hockstein and Dr. Paula Ko are retina specialists at Eye Physicians and Surgeons who are committed to helping patients with AMD and other retinal diseases. If you would like to learn more about AMD or to
schedule an appointment call (302) 652-3353.
1207 North Scott Street, Wilmington, DE 19806