Age Related Macular Degeneration
By Dr. Carolyn Glazer-Hockstein
Age-related macular degeneration (AMD) affects millions of Americans and can cause them to lose their central vision.
AMD is a degenerative disease of the macula, a part of the retina which controls a person’s central vision. Symptoms can start with distortion of straight lines or missing parts of letters but can lead to a dark spot in the center of the vision causing complete loss of central vision. Patients will never go completely blind from this disease but they can become “legally blind” from loss of central vision. They can lose the ability to do things like drive, recognize friends’ faces, read and write legibly.
There are 2 types of AMD, the dry and the wet form. The dry form is characterized by little yellowish deposits in the macula called drusen. These are “aging spots” that accumulate from by-products of retina metabolism. Unfortunately there still is no treatment for dry AMD.
In contrast, the wet form of AMD is characterized by abnormal blood vessels that grow underneath the retina. Twenty percent of patients have wet AMD but these patients make-up 80% of the people who have significant vision loss. Patients with wet AMD can experience sudden vision loss when these abnormal blood vessels start to leak or bleed. This type of vision loss occurs over days to weeks and inevitably gets worse if not treated.
Intraocular injections are successfully being used to treat wet AMD. These injections not only stabilize but can improve vision. They are given indefinitely to a patient off and on for the rest of a patient’s life.
Intra-ocular Avastin (Genentech $60) injections can be given monthly. It has been shown to stabilize or improve vision in about 90-95% of patients. Currently this drug is being used off-label as this drug was FDA approved for colon cancer, not for use in the eye.
Intra-ocular Lucentis (Genentech $1,950) is another drug that successfully treats wet AMD. Lucentis is FDA approved for treatment of wet AMD. Both drugs are vasoendothelial growth factor (VEGF) inhibitors and work by causing abnormal blood vessels to regress.
A recent study (CATT trial) funded by the NIH compared the efficacy of Avastin and Lucentis. This large prospective randomized study showed that Avastin and Lucentis were equally effective in preventing vision loss and improving vision in patients who were followed monthly.
However, there was a trend toward Lucentis drying out the retina better and having a slightly lower post-injection hospitalization rate for
systemic complications.
In addition there have been a small number of site-threatening infections in patients receiving Avastin. This may have occurred because of possible contamination during the compounding process that occurs when Avastin is used.
Clinically, Avastin and Lucentis are equally effective, but they are different drugs and behave differently when given to a patient. It is vastly important for the retina specialist to have the ability to choose which drug (and switch between the two if appropriate) to use on a patient with wet AMD. They are both good tools to use in successfully treating wet AMD.
Anti-vascular endothelial growth factor (VEGF) inhibitors Avastin and Lucentis have revolutionized the way we care for patients with age-related macular degeneration. Prior to VEGF inhibitors, treatment was limited to thermal laser and photodynamic therapy (PDT). Unfortunately, even with treatment, many patients with AMD became legally blind garnering only modest visual improvement with laser or PDT treatment. With the use of Avastin and Lucentis, the diagnosis of AMD no longer means eventual and certain blindness.
“VEGF Trap” is now a new weapon in our armamentarium against AMD. This unique molecule may have advantages over Avastin and Lucentis in that it has a higher binding affinity for VEGF and longer half life than the currently used VEGF inhibitors. This means that the time between injections may be longer than what we see in Avastin and Lucentis.
Multiple clinical trials have demonstrated VEGF Trap’s equivalence to Lucentis. Adverse events in all treatment groups were also equivalent so it is felt that this new drug is at least equally effective and safe. The critical results of this trial demonstrated that VEGF trap may reduce the treatment burden for patients and families regarding frequency of intra-ocular injections.
VEGF trap has the same ability to deliver outstanding visual results and may require less frequent dosing than Lucentis and Avastin. It is a hopeful time for many AMD patients as new therapies become available.
SYMPTOMS OF WET AMD
• Acute central vision loss
• Acute distortion in vision
• Unexplained vision loss in someone with dry AMD
Call your eye care provider if you have any of these above symptoms, as they may be the beginning signs of AMD.
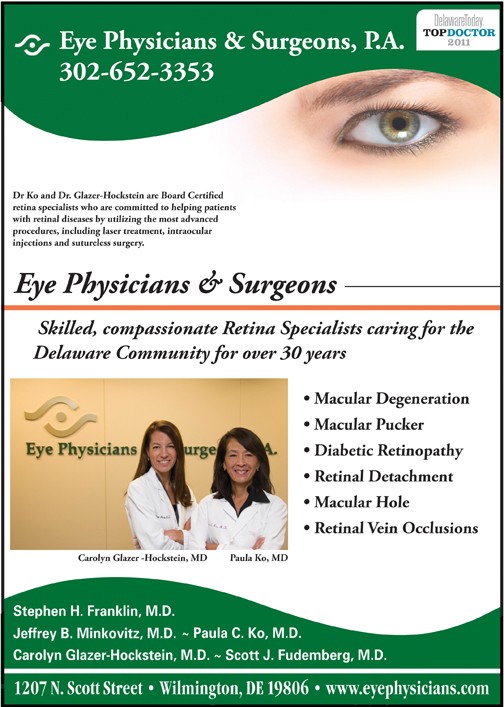
Dr. Carolyn Glazer-Hockstein and Dr. Paula Ko are retina specialists at Eye Physicians and Surgeons who are committed to helping patients with AMD and other retinal diseases. If you would like to learn more about AMD or to schedule an appointment call (302) 652-3353.
Dr. Glazer-Hockstein graduated Cum Laude from Jefferson Medical College. She was a member of the Hobart Armory Hare Honor Medical Society and was elected to the Alpha Omega Alpha Honor Society. She also received the Carol R. Mullen prize in ophthalmology. She completed her residency at the Scheie Eye Institute, University of Pennsylvania. During that time she was elected Chief Resident. After residency, Dr. Glazer-Hockstein completed a two years medical retina fellowship at the Scheie Eye Institute, University
of Pennsylvania.
Dr. Glazer-Hockstein has published multiple articles in peer-review journals and has lectured on a variety of retinal disease subjects. Her specialization includes but is not limited to: macular degeneration, retinal vascular disease, and diabetic retinopathy.
Paula C. Ko, MD is with Eye Physicians & Surgeons, P.A., 1207 North Scott Street, Wilmington, DE 19806. Dr. Ko graduated with honors from the Ohio State University College of Engineering in 1984. Dr. Ko received her M.D. degree from the Ohio State University College of Medicine in 1989, again with honors. Following her residency in Ophthalmology at Temple, Dr. Ko served a prestigious fellowship at Georgetown University in diseases of the retina and vitreous, and is Certified by the American Board of Ophthalmology.
Dr. Ko has an area of special expertise in retinal problems, especially diabetic eye disease, macular degeneration, retinal detachment, and CMV retinitis. Dr. Ko has lectured extensively, and has published many papers on these topics. Dr. Ko is active in resident training, and is on staff at the University of MD and Temple University, as well as at the Medical Center of DE. Dr. Ko is at the forefront of ophthalmic technology, and utilizes the most advanced procedures, including laser treatment and intraocular injections, in the care of her patients.