A New Drug For Wet AMD-2
By Dr. Paula C. Ko
Wet AMD is the leading cause of blindness in the United States for people over the age of 65. Patients develop abnormal blood vessels that grow underneath the macula (central part of the retina) which leak and bleed. This can take away central vision which is used for things like reading, recognizing people’s faces and driving. For the last 10 years we have been successfully treating people with wet AMD using injections in our office on a monthly basis. Some patients are lucky and can go as long as every 2 or sometimes every 3 months for their injections. The frequency of injections are based on how long the drug remains active in the eye. The drugs available today treat but do not cure and are active for only about 4-8 weeks. Once their efficacy wears out, leaking and bleeding restarts and patients can lose vision again, so patients will need injections indefinitely. Drugs available today that treat wet AMD include Avastin, Lucentis, and Eylea. Lucentis and Eylea are very expensive and represent a large cost to the Medicare system.
Intraocular injections have revolutionized our ability to treat wet AMD. But, as successful as they have been, they come at a price of time and cost. First, there are very many patients in the United States with this disease. Patients are living longer and one of the main risk factors is age. Much time is spent by the patient and their family to get these injections. As a busy retina specialist my schedule is packed full of patients that need these injections for wet AMD as well as for diseases like diabetic retinopathy, diabetic macular edema, vein occlusions, and cystoid macular edema. Finding a new drug that lasts longer will help decrease the treatment burden, and in October of this year, this drug may be FDA approved.
Brolucizumab is an anti-VEGF drug that works against VEGF (Vascular Endothlial Growth Factor) by stopping its ability to cause abnormal blood vessel formation. The other drugs we use now work similarly but each drug is a different size and blocks different chemical pathways. Brolucizumab is a humanized antibody fragment that also blocks the effects of VEGF. Because it is a fragment of an antibody, it’s molecular weight is very low which allows a higher concentration of the drug to be injected into the eye. Being a small fragment also allows it to penetrate tissue more easily and remain in the tissue longer, which ultimately makes the drug remain active longer. Clinically, what that means is that instead of an average patient getting an injection every 4 weeks, they will now get one every 12 weeks. Some patients who come in every 2-3 months for an injection may be able to get an injection every 6 months.
This drug is projected to be FDA approved in October of this year. The remaining unknown is the cost. Although time will be saved with diminishing the treatment burden on patients and their families, the cost of the drug most likely will be very high. Currently the drug prices range between $70 – $1800 per vial for our current drugs available. We will soon find out the cost of this highly anticipated drug.
Bios
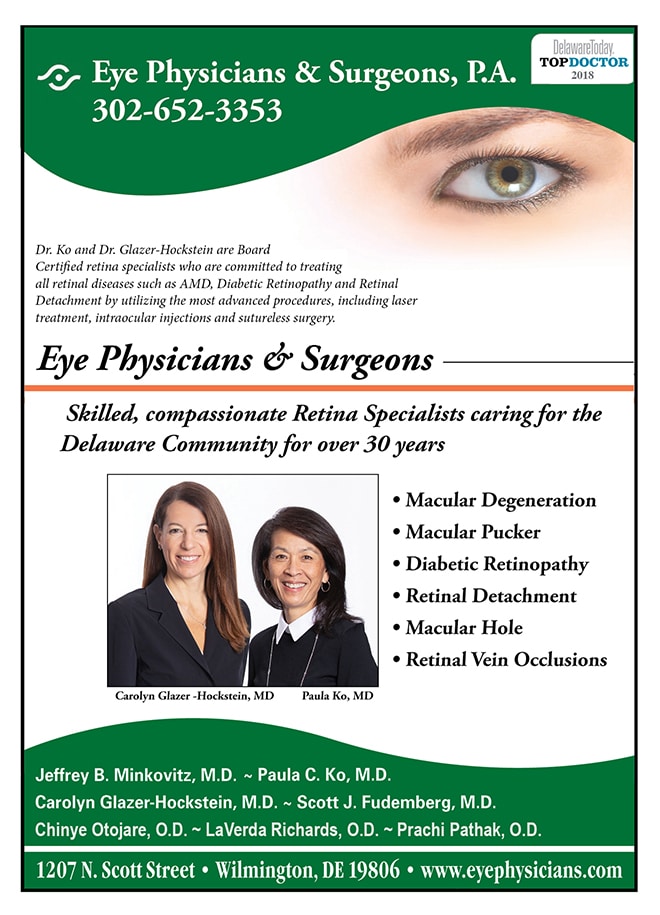
Dr. Glazer-Hockstein graduated Cum Laude from Jefferson Medical College. She was a member of the Hobart Armory Hare Honor Medical Society and was elected to the Alpha Omega Alpha Honor Society. She also received the Carol R. Mullen prize in ophthalmology. She completed her residency at the Scheie Eye Institute, University of Pennsylvania. During that time she was elected Chief Resident. After residency, Dr. Glazer-Hockstein completed a two years medical retina fellowship at the Scheie Eye Institute, University of Pennsylvania.
Dr. Glazer-Hockstein has published multiple articles in peer-review journals and has lectured on a variety of retinal disease subjects. Her specialization includes but is not limited to: macular degeneration, retinal vascular disease, and diabetic retinopathy.
Dr. Ko graduated Cum Laude from the Ohio State University College of Engineering and received her M.D. degree from the Ohio State University College of Medicine, with honors. Following her residency in Ophthalmology at Temple, Dr. Ko served a prestigious fellowship at Georgetown University in diseases of the retina and vitreous and is Certified by the American Board of Ophthalmology.
Dr. Ko’s area of expertise is in retinal problems, especially diabetic eye disease, macular degeneration, and retinal detachment. She lectures extensively and has published many papers on these topics. Dr. Ko is active in resident training and is on staff at Temple University, as well as at the Medical Center of DE. She is at the forefront of ophthalmic technology, and utilizes the most advanced procedures, including laser treatment, suture-less surgery and intraocular injections, in the care of her patients.