Functional Medicine & Non-Alcoholic Fatty Liver Disease

By Dr. Cynthia Crosser
Have you ever been told that you have or are in danger of developing NAFLD? If you are in this position, don’t take this lightly. Please do something! This condition includes NAFL and NASH which are largely silent diseases and are associated with conditions such as obesity, metabolic syndrome, and Type 2 diabetes. NAFLD is correlated with cardiovascular disease, the number one cause of mortality in the US. It is estimated that as much as half of Americans are suspected of having silent NAFLD.
While this is a sequence of physiological changes, the key component is the accumulation of fat in liver cells in the absence of alcohol consumption, autoimmune disease, or viral infections. This results in the production of inflammatory chemicals such as cytokines that promote insulin resistance. Serum free fatty acids (FFAs) increase and when the liver can no longer clear these FFAs, triglycerides become stored in the liver cells. When this occurs the liver also becomes susceptible to the damage caused by environmental chemicals and an imbalanced microbiome (gut dysbiosis). Many drugs, parabens, phthalates, and bisphenols (from plastics) trigger obesity, further driving this process. The widespread use of high fructose corn syrup has been a major player in this scenario, a contributor to the obesity epidemic, especially in children. Microbial dysbiosis is a potent initiator and contributor to NAFLD. Although alcohol is not the driver of NAFLD, it will cause cellular insult. Drinking 1-4 alcoholic beverages per day overwhelms the natural detoxification and metabolic regulation that a healthy liver can accomplish.
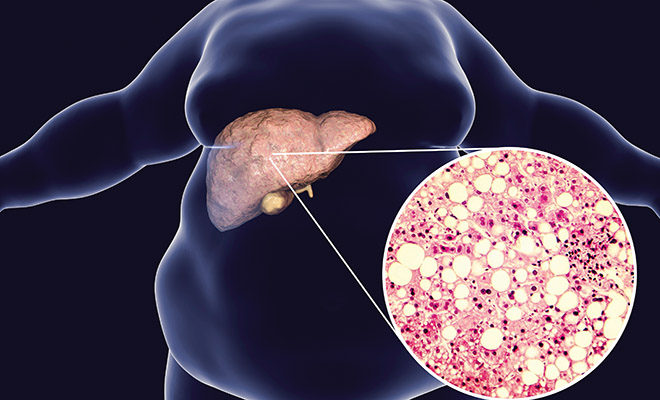
The diagnosis includes laboratory markers such as ALT, AST, GGT, triglycerides, HDL, adiponectin, and fasting insulin as well as a liver biopsy.
Enter uric acid into this story. Most often I will not see uric acid ordered on bloodwork in conjunction with the lipid panel. This is not only a biomarker for NAFLD, but also a causative factor. When uric acid goes up, so does the risk of hypertension. And this high uric acid also correlates back to HFCS and foods high in purines. High uric acid correlates with high CRP, a cardiac inflammatory marker. Salt adds to the metabolic nightmare. A 2018 study of 13,000 healthy adults showed that a high-salt diet (>11 grams/day) predicts the development of diabetes AND NAFLD!
So how do we address this. Lifestyle changes are absolutely critical to include exercise, reduction of dietary carbohydrates, reduction of environmental toxins, restoring your gut microbiome, avoiding processed foods, reducing alcohol consumption and monitoring your serum uric acid levels on a regular basis. And suffice to say that a low-carb diet is not a high-fat diet. A moderate to high-carbohydrate diet with some fat will cause increased fat storage and eventually will produce inflammation, insulin resistance and fatty liver. These approaches can assist in weight loss which will reduce the triglyceride stores, reversing the inflammatory cascade and restoring metabolic flexibility.
This is a doable process and, as we’ve always heard . . . You get out of it what you put into it! For more information, please contact us at
Bio
Cynthia Crosser is a Doctor of Chiropractic and a Fellow with the International Academy of Medical Acupuncture. She completed two postgraduate programs: Chiropractic Neurology and Physical Rehabilitation. She is currently in the process of certification with the Institute for Functional Medicine.
For more information, contact us at 302-994-1010 or through our website at www.crossernaturalhealth.com
Wellness within reach!
Pike Creek 302-994-1010
5700 Kirkwood Hwy., Suite 101, Wilmington, DE 19808
www.facebook.com/crossernaturalhealth
www.facebook.com/CrosserChiroThin
Chiropractic, Acupuncture, Weight loss, Neurofeedback, Nutritional Counseling

