“Ask Your Doctor Today If This Medication Is Right For You…”
By Robert M. Carroll, M.D.
This familiar phrase is one we have all heard as part of the seemingly endless pharmaceutical advertisements that bombard our daily lives. Whether it is a sign on the side of a public bus, a commercial during daytime television, or a video on our smart phone, we are inundated with information about the newest medications. This is for good reason: over four billion prescriptions are filled in the United States every year, and many of these advances have changed public health for the better. Increased systemic medication use is not without risk, though, and understanding how some of these drugs may affect our vision is critically important.
Hydroxychloroquine (brand name Plaquenil) is a medication initially created to prevent malaria but is now most commonly used to treat autoimmune conditions such as rheumatoid arthritis or lupus. While it works well for many patients, it also carries a low, but serious, risk of central vision loss. Chronic use of hydroxychloroquine can lead to toxicity of the retina, the thin layer of tissue that lines the inside of the eye and carries the signals to make the images that we see. There is about a 1-2% chance of developing toxicity from this medication over the first 10 years of use, but that risk can increase significantly with longer duration. Patients have no symptoms with early toxicity, and the American Academy of Ophthalmology has recommended screening exams for all patients taking hydroxychloroquine. If you are on this drug, a retina specialist should examine you and use special testing to determine if there are signs of retinal toxicity.
Pentosan polysulfate (brand name Elmiron) is a medication used to treat interstitial cystitis, a painful condition that primarily affects women with symptoms of chronic urinary urgency, frequency, and pelvic discomfort. In 2018, retina specialists at Emory School of Medicine discovered a pattern of abnormal retina findings in patients taking pentosan. These patients complained of blurry vision, difficulty reading, and trouble adapting to dark environments. Many had findings easily confused for age related macular degeneration, but special retinal imaging tests revealed unique manifestations associated with this medication. There is now a clearly identifiable risk of retinal toxicity with pentosan, primarily linked to long-term use and high doses. All patients who have taken pentosan should have a dilated eye exam and retinal imaging performed by a retina specialist.
Semaglutide (brand names Ozempic and Wegovy) is a popular medication with great outcomes in the treatment of diabetes and obesity. While it was being approved, one of the many clinical trials found an association with worsening of diabetic retinal disease in patients who had diabetic retinopathy. Due to this, semaglutide carries a warning that patients with diabetic retinopathy may experience vision issues and should have their eyes examined while on the medication. One possible explanation for this finding is a phenomenon already known for decades where diabetic retinopathy temporarily worsens with rapid blood sugar control. Fortunately, these changes typically reverse themselves and in general, good blood sugar regulation is the best thing a diabetic patient can do to protect their vision. More recently, researchers from Harvard Medical School reported a potential association with semaglutide and ischemic optic neuropathy, a specific type of eye stroke that can cause significant vision loss. Their work does not imply any direct causation from the medication, but more investigation is warranted. There is yet to be definitive proof that semaglutide can make diabetic eye disease worse or cause vision loss. However, the consensus of many retina specialists is that patients who are taking semaglutide should have a dilated eye exam and it may be necessary to follow you more closely.
We are fortunate to live in an age where rapid scientific advancements allow many of us to live longer, healthier lives. It is important to remain informed about potential risks of medications, though, especially as it pertains to your vision. You should always speak with your prescribing medical provider if you have questions about any medication you are taking, and they can refer you to an eye care specialist for an evaluation. If you are taking any of the medications reviewed in this article and would like to schedule an appointment with a retina specialist at Eye Physicians and Surgeons, please call 302-652-3353 or visit www.eyephysicians.com.
follow us on facebook & instagram
Bio
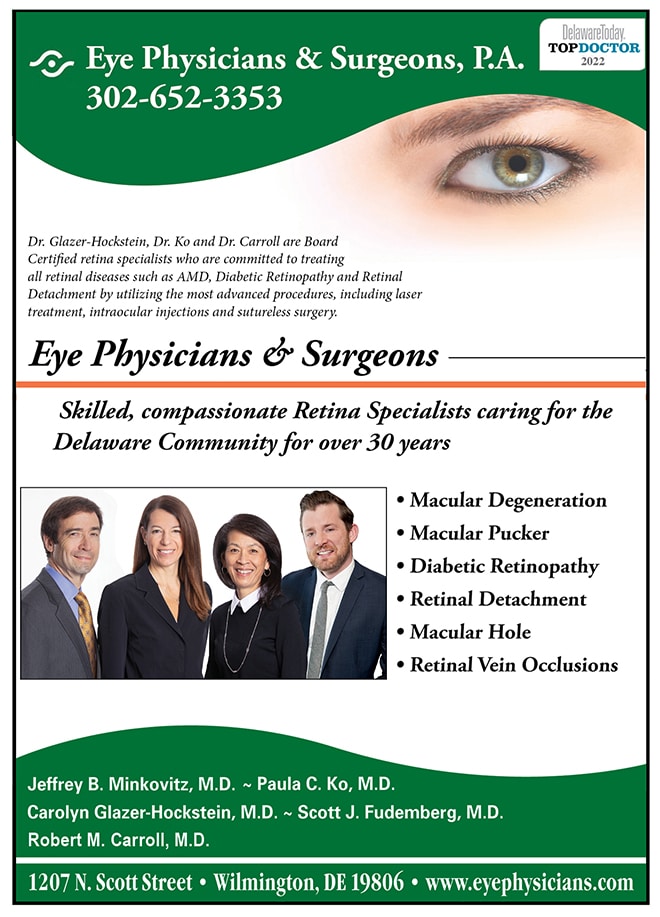
We are very excited to announce our newest retina specialist at Eye Physicians and Surgeons, Dr. Robert Carroll. Dr. Carroll is a board-certified, fellowship-trained vitreoretinal surgeon who specializes in the care of diabetic retinopathy, age related macular degeneration, retinal vascular disease, and posterior uveitis as well as small-gauge sutureless surgical repair of retinal detachment, macular hole, complex diabetic pathology, and secondary intraocular lenses.
Dr. Carroll completed his undergraduate degree in biochemistry with honors at the University of Notre Dame and earned his medical degree at Rutgers-Robert Wood Johnson Medical School. He completed his internship at Albert Einstein Medical Center in Philadelphia, residency in ophthalmology at Mount Sinai Hospital in New York, and fellowship in vitreoretinal surgery at the Scheie Eye Institute of the University of Pennsylvania, where he was awarded the Fellow Excellence in Teaching Award.
Please join Eye Physicians and Surgeons in welcoming Dr. Carroll to our practice!