Retinal Vascular Disease – Retinal Vein Occlusion
By Dr. Carolyn Glazer-Hockstein
An ancient proverb states “the eyes are the windows of the soul.” As ophthalmologists, the eyes are our window to the body’s circulation system. We see changes in the blood vessels of the retina that reflect what is occurring throughout the body. The retina is a thin sheet of nerve tissue in the very back of the eye. It has its own distinct blood supply and is one of the most metabolically active tissues in the body. The retina is extremely sensitive to changes that occur in blood vessels. Patients with common medical problems like high blood pressure and diabetes may develop loss of vision. This is related to the changes in blood flow through the retina that these diseases can cause. One of the most common retinal blood vessel diseases (or retinal vascular diseases) is a retinal vein occlusion.
Retinal vein occlusion occurs because the veins in the retina become clogged or blood flow becomes interrupted. This blockage can result in permanent damage to the retinal veins. Most often a “thrombus” or blood clot causes the blood vessel occlusion. Patients experience painless vision loss from lack of blood flow to the retina, also known as “ischemia.” Another significant cause of vision loss is “macular edema” or swelling in the center of
the retina.
Risk factors for the retinal vein occlusions include high blood pressure, high cholesterol, atherosclerosis, blood clotting disorders, and inflammatory diseases. People 50 to 60 years old are most commonly affected.
Treatment of retinal vein occlusion begins by controlling any underlying medical problems. It is important for patients to maintain good blood pressure and cholesterol control. Patients with underlying clotting disorders may need to see a hematologist.
While it is important for patients to optimally control their medical problems, there are several new treatments which can be targeted at the retina to help patients maintain their best possible vision. Treatments which specifically target the retina are important because no oral medications or eye drops help patients with retinal vein occlusions.
Until recently, laser therapy was the only treatment for retinal vein occlusion. Laser therapy can decrease swelling within the retina which help to preserve vision and in some patients can result in visual improvement. Newer treatments include injections of medicine into the vitreous cavity (the gelatinous space in the eye). The most commonly used medications include steroids and vascular endothelial growth factor inhibitors (VEGF inhibitors). VEGF is a protein that is abnormally high in the eye of patients with retinal vein occlusions. It causes abnormal new blood vessel growth (neovascularization) and causes blood vessels to leak fluid into the retina resulting in blurry vision. Patients typically require a series of anti-VEGF injections every four to six weeks. Another injectable medicine is triamcinolonc, a steroid which is very effective in decreasing swelling and blood vessel leakage within the eye. Osurdex is a longer acting steroid implant which can also be used to treat retinal vein occlusions. The Osurdex implant is inserted into the eye in the office under local anesthetic and can be effective
in the treatment of retinal vein occlusions.
During the past few years many patients have benefited from these treatments for retinal vascular disease. With the new powerful arsenal of intravitreal medications, retinal specialists not only preserve vision but allow maximum visual outcomes. Treatment may require ongoing care but with these new therapies, we can help to prevent blindness.
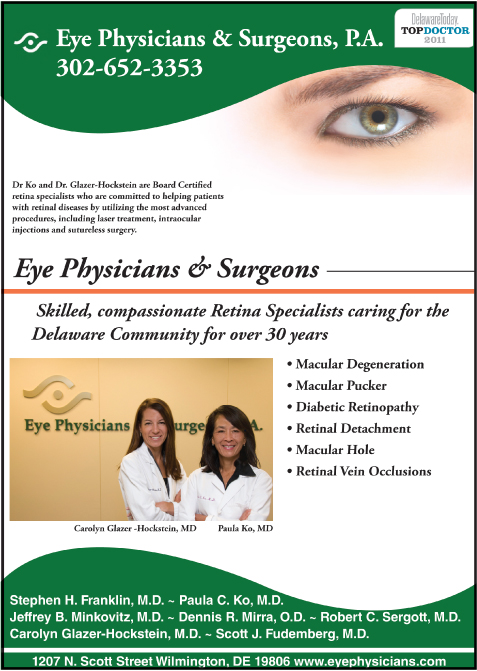
Dr. Glazer-Hockstein graduated Cum Laude from Jefferson Medical College. She was a member of the Hobart Armory Hare Honor Medical Society and was elected to the Alpha Omega Alpha Honor Society. She also received the Carol R. Mullen prize in ophthalmology. She completed her residency at the Scheie Eye Institute, University of Pennsylvania. During that time she was elected Chief Resident. After residency, Dr. Glazer-Hockstein completed a two years medical retina fellowship at the Scheie Eye Institute, University
of Pennsylvania.
Dr. Glazer-Hockstein has published multiple articles in peer-review journals and has lectured on a variety of retinal disease subjects. Her specialization includes but is not limited to: macular degeneration, retinal vascular disease, and diabetic retinopathy.
Paula C. Ko, MD is with Eye Physicians & Surgeons, P.A., 1207 North Scott Street, Wilmington, DE 19806. Dr. Ko graduated with honors from the Ohio State University College of Engineering in 1984. Dr. Ko received her M.D. degree from the Ohio State University College of Medicine in 1989, again with honors. Following her residency in Ophthalmology at Temple, Dr. Ko served a prestigious fellowship at Georgetown University in diseases of the retina and vitreous, and is Certified by the American Board of Ophthalmology.
Dr. Ko has an area of special expertise in retinal problems, especially diabetic eye disease, macular degeneration, retinal detachment, and laser and intraocular injections. Dr. Ko has lectured extensively, and has published many papers on these topics.
Dr. Ko is active in resident training, and is on staff at the University of MD and Temple University, as well as at the Medical Center of DE. Dr. Ko is at the forefront of ophthalmic technology, and utilizes the most advanced procedures, including laser treatment and intraocular injections, in the care of her patients.
Dr. Carolyn Glazer-Hockstein and Dr. Paula Ko are retina specialists at Eye Physicians and Surgeons who are committed to helping patients with AMD and other retinal diseases. If you would like to learn more about AMD or to schedule an appointment call (302) 652-3353.